2017 Greater Value Portfolio Awards
Donaghue is pleased to announce its four Greater Value Portfolio awards for 2017. Since the program began in 2015, $6.4 million has been invested in research that demonstrates new approaches to improved health care value (the Rx Foundation provided a portion of this investment for the 2016 awards).
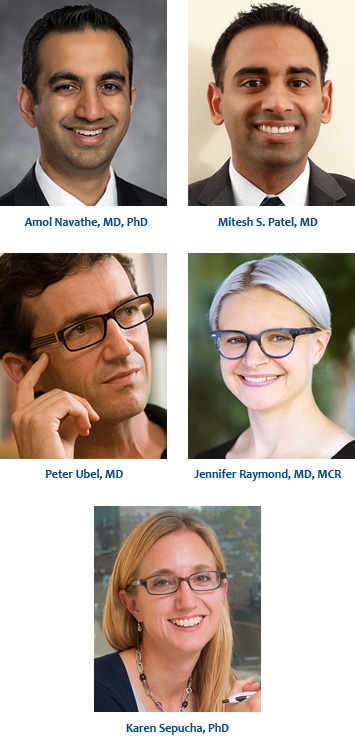
Amol Navathe, MD, PhD Mitesh S. Patel, MD
The University of Pennsylvania
Project Cost – $593,108
The REDUCE Trial‐ Randomized trial of EHR Defaults and Using social Comparison feedback to Effectively decrease opioid prescription pill burden
Opioid‐related abuse and overdose represents a growing national epidemic in the United States. Physician practice patterns play an important role; opioid prescriptions impact the likelihood that patients will misuse or become dependent on these medications, with longer prescriptions leading to greater sustained use. The objective of this study is to conduct a pragmatic randomized, controlled trial to evaluate the effect of two scalable behavioral economics approaches to reduce physician opioid prescribing. The different methods being compared are the impact of instituting an electronic health record default option for the number of pills per opioid prescription and providing monthly social comparison feedback to physicians on opioid prescribing patterns — both methods will be compared individually and in combination. The trial will use a one‐year pre‐intervention period and then a one‐year intervention period at Sutter Health System in 58 emergency department and urgent care sites throughout the Western U.S.
Peter Ubel, MD
Duke University
Project Cost – $599,862
Examining Best Practices for Factoring Out-Of-Pocket Expenses into Patients’ Health Care Decisions
The goal of this project is to examine best practices for difficult cost conversations between physicians and patients with the focus being on patients with serious illness who are experiencing financial distress from healthcare costs. The study will primarily be qualitative and observational. It will involve physicians who spend the majority of their time providing clinical care affiliated with Duke University and the University of Pennsylvania. Forty physicians, each of whom will interact with six patients, will be recruited for a total of 240 observations.
Jennifer Raymond, MD, MCR
Children’s Hospital Los Angeles
Project Cost – $590,701
CoYoT1 to California (CTC) – Telemedicine to Engage Young Adults with Diabetes
As more individuals from diverse ethnic and racial backgrounds are diagnosed with Type 1 Diabetes (T1D), there is a concomitantly escalating need to address the disparities in diabetes outcomes in these populations. Although young adulthood is a challenge for all patients with diabetes, minority and low socioeconomic young adults face have even more obstacles to ideal management. Due to poor outcomes in this population, there is an imminent need for alternative care models to improve engagement of young adults with T1D in clinical care and address the barriers to improved health outcomes. This study will adapt the previously established, successful combination of telemedicine and shared medical appointments, “CoYoT1 Clinic” (Colorado Young Adults with T1D), to the Southern California young adult population. Using meticulously designed study methods involving patient advisors, quantitative and qualitative data collection, collaboration with local stakeholders, intervention development, and patient randomization to telemedicine or in-person clinical visits, we will address the needs of high-risk young adults in Southern California, with the goals of increasing access to care, improving follow-up frequency, and strengthening patient and provider satisfaction.
Karen Sepucha, PhD
Massachusetts General Hospital
Project Cost – $599,997
Matching the right person to the right treatment: Shared decision making for high cost elective procedures
Studies have shown large gaps in the quality of medical decisions. In cases of elective surgery, poor quality decisions result in low value care with worse outcomes and higher costs. The proposal will examine whether routine measurement of shared decision making for elective surgery decisions with feedback to clinicians and administrators has the potential to improve the value of care provided to patients. The aims of this proposal are to (1) integrate new performance measures to assess shared decision making for elective orthopedic procedures, (2) explore how the data may be used to motivate practices to increase rates of informed, patient-centered decisions, and (3) examine the impact on high value care. The study focus is on knee or hip replacement for osteoarthritis and surgery for herniated disc or spinal stenosis because of their high cost, prevalence, and variation in utilization. In the first year, about 600 patients will be surveyed using well-validated instruments to assess the rate of informed, patient-centered decisions. This type of patient-reported performance measurement is new, and we plan to engage stakeholders (primary care, specialists, nursing, patients, and administrators) in the process. Working with these stakeholders, we will explore the implications of the data, identify high and low performers to target for additional qualitative data collection, and generate insights into best practices. In the third year of the study, 600 new patients undergoing the same procedures will be surveyed to examine whether providing feedback impacts value, including health outcomes and costs across our system.