Choosing Wisely® Proposes “Less” and “More” – Reducing Low-Value Care While Increasing Health Equity
March 13, 2020
Kelly Rand is a Program Officer at the ABIM Foundation. In this role, she oversees activities related to a major grant the ABIM Foundation has received from the Robert Wood Johnson Foundation® (RWJF) to fund the expansion of the Choosing Wisely® campaign.

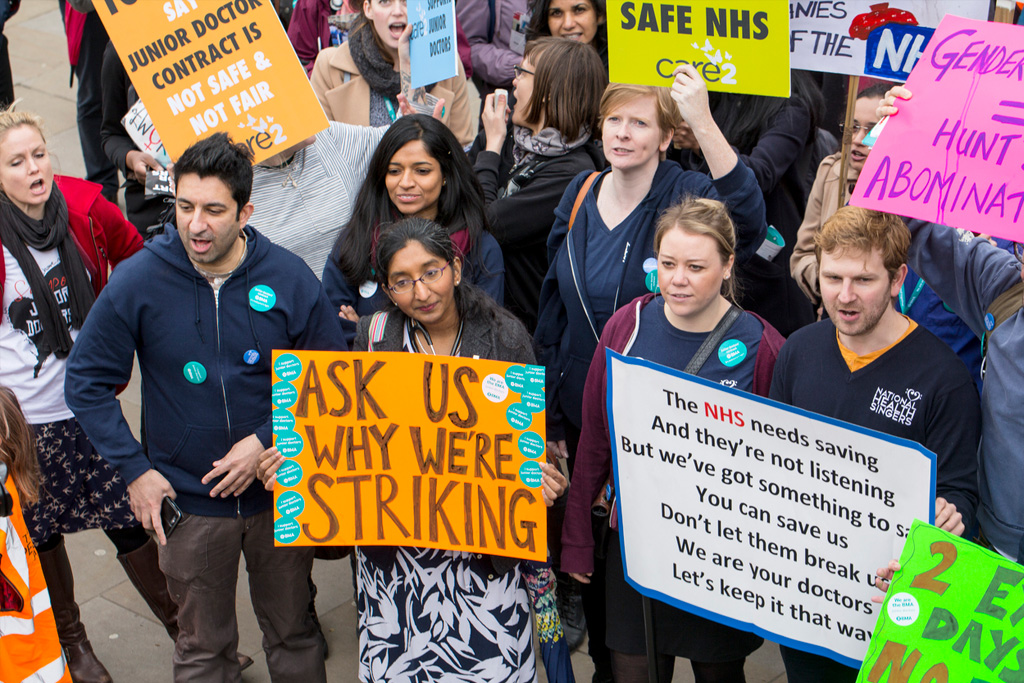
The cost of American health care is a problem for patients. More than one in four Americans report difficulty paying their medical bills. Increased costs to patients has been shown to negatively affect patients to fulfill their patient plans for treatments and care, reduce access to care and increase mortality. Even patients who may not have high out of pocket direct medical costs report concerns about transportation, lost income, extended time spent at visits, child care issues and myriad related indirect costs of care. Through ABIM Foundation’s Choosing Wisely campaign, we’ve focused on helping clinicians and patients have better conversations about the overuse of tests and treatments and to support clinician efforts to help patients make smart, effective choices. Overuse, or care that has a greater potential for harm than benefit, is widespread in American medicine, with severe effects on both quality of care and health care costs.
Woven throughout the public discourse on overuse is the equally concerning issue that one-third of Americans either have no insurance or inadequate insurance. With this concern, some voices suggest we should tackle access to care issues rather than focusing on overuse. Perhaps a better solution is to integrate overuse and underuse efforts and design these efforts with a health equity lens. Several studies have found that low-value care is common among patients without insurance or with Medicaid, and that physicians practice similar rates of low-value and high-value care regardless of their patients’ insurance status. Plainly said, patients who have access issues may be less likely to receive the care they need and more likely to receive care that has potential for harm.
What we are doing right
The keystone of Choosing Wisely has always been the clinician-patient conversation. Engaging patients in conversations about preferences and goals, providing patient education materials at appropriate literacy levels and encouraging patients to ask questions with tools such as the “5 questions to ask your doctor before you get any test, treatment or procedure” are all powerful ways to help clinicians and patients determine appropriate care.
Through focus groups with patients, ABIMF has learned:
- While about half of the participants initially thought “more care is better,” learning that one out of every four or five tests, treatments or procedures doctors order for their patients ends up having no benefit made them question their beliefs and prompted several participants to share stories of harm they experienced from overuse.
- Focus group participants are comfortable challenging their doctors about care decisions.
- Participants said they conducted fairly extensive research about treatment options and trusted their own judgment about what’s best for them.
- More than anything, low-income focus group participants wanted to be heard by the health care system.
- When having conversations about potential overuse and appropriate care, patients want a clear rationale for recommendations – including explaining potential harm – and recognition that there was a comprehensive plan in place.
- Focus group participants feel empowered by the Choosing Wisely mission and want a health system that recognizes the individual needs of patients.
Focusing resources on preparing both clinicians and patients to have better conversations can include:
- communications training for clinicians on how to have difficult conversations;
- communications training with patients;
- dissemination of patient materials at appropriate literacy levels that discuss when care is and is not needed and when you might wait; and,
- adjustments to clinical workflows so that preparatory conversations can be had with different members of the care team.
There is still room for improvement in clinician-patient communications even in organizations committing resources to improving them. Focus group participants expressed relatively low levels of trust in their providers, and some participants believed their clinicians displayed bias in ordering (and not ordering) tests or treatments for them. Additional training on cultural humility can help the care team, and more research is needed about how to create a question-friendly environment for patients. Working with trusted community-based organizations to educate patients is an additional way to add the patient voice to high value care efforts and help provide trustworthy, accurate information to patients.
Where we need to do more
Most overuse reduction projects focus explicitly on overuse and we measure their success by volume reduction. Quality improvement professionals need to move to more sophisticated approaches, and design high value care implementation projects that are designed to focus on appropriateness of care. For example, because African Americans have a disproportionate burden of cancer, efforts related to cancer screening should work simultaneously to reduce unnecessary screenings and increase appropriate screenings. This type of project requires targeted communications, and measurement must include a breakdown of the populations affected with goals for increases and decreases rather than a straight volume reduction.
Additionally, balancing measures can be added to underuse projects to heighten patient safety. For example, if your setting is working on stricter control of A1c in diabetic patients, a balancing measure could be added to ensure that older adults who are at greater risk of falls from hypoglycemia have adjusted A1c goals.
While reducing overuse of tests and treatments is a worthy endeavor, these efforts must be balanced with protections against increasing health inequities. Choosing Wisely can engage patients and health care providers in meaningful conversations and improve appropriateness of care, but in order to do that we must be strategic in our communications and our implementation design.
If you are interested in learning more about the focus groups mentioned above, please read Communicating About Overuse with Vulnerable Populations.
Back Issues

Developing a Research Agenda on High-Value, Equitable Care: The Power of Being Practical, Inclusive, and Innovative