What COVID-19 Has Exposed About Racism in Health Care and How We Can Work Toward a Solution
June 16, 2020
President, Universal Health Care Foundation of Connecticut

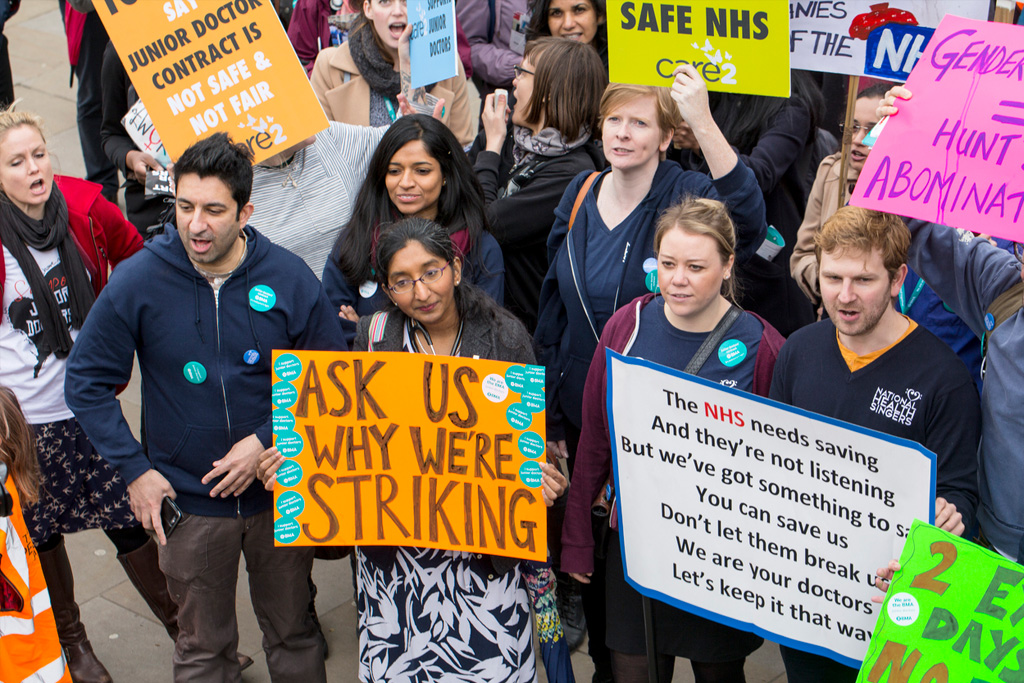
Over the past few months, our systems have shown their true colors. Black people in the U.S.A. are dying at the hands of our health care system and justice system. Some are just beginning to realize these injustices, but many have been aware of them for a long time.
On June 4 we held an online discussion, “Racism and Health Care: What COVID-19 Has Exposed” to begin to unpack how racism in health care produces worse health outcomes for Black and Brown communities — and what we can do about it.
Where does this story begin?
A friend of Universal Health Care Foundation of CT once said, “Racism is a public health pandemic.” At its core, this statement recognizes how racism has influenced our many systems and institutions for over 400 years, and is at the root of disparities for Black and Brown people.
Denise Smith, founding Executive Director of the National Association of Community Health Workers, joined us for the discussion. She reminded us of the long history of racism in this country, starting in 1619 with the arrival of the first slave ships. Connecticut, she said, was late to abolition.
Racism in health care today is at the root of Black and Brown communities experiencing wide health disparities relative to their White counterparts. Racism does not only impact health care delivery, it also impacts other factors that influence health, like socioeconomic status, education, housing, employment, and many more. “If we don’t deal with the scourge of racism, we won’t chip away at our individual missions around health equity and social justice,” she said.
Is anything being done about this?
There are health care providers everywhere who are actively trying to bridge these gaps. Asher Delerme, Executive Director of Chemical Abuse Services Agency, Inc. (CASA), also joined us and told the story of his organization, which is set up to address some of these health inequities by meeting the needs of Black and Brown communities.
He said his organization has struggled during the COVID-19 pandemic, citing a congregate living program that serves patients with HIV. Despite programs like these having a high need for COVID-19 testing, Delerme said it was difficult to secure.
Delerme had to advocate for his program to get the testing and care they needed. “Unless you’re rich or a politician, you’re not going to get tested,” he recalled being told at a community health center. Ultimately, he was able to get the testing they needed, but not without tireless advocacy.
But this isn’t an isolated example of available care being denied because of bias. Dr. Julian Nieves, a practicing physician at UConn Health, shared similar experiences.
He recalled a Black man at his facility who was suffering from a heart attack and didn’t get the care he needed right away because of suspicions of him having COVID-19. Dr. Nieves pointed out that this is a deviation in the standard of care, and he wondered if it would have been different had it been someone else who came in having a heart attack.
This crisis is exacerbating health inequities. Some examples are through language barriers, access to care, access to telehealth, and transportation problems. This is all without even mentioning implicit bias, which Dr. Nieves explained plays a part even when doctors think they are treating patients equally.
What more can we do?
We have to get beyond talk. What are potential solutions to eliminate or mitigate racism in the health care system? Community health workers, recovery coaches, and doulas are critical to addressing health disparities, which are rooted in racism.
As Dr. Nieves pointed out, it is also important for us to be talking to each other and having these difficult discussions to identify solutions. Delerme noted the importance of confronting ourselves, our institutions, our policies, and our leaders and how all of these contribute to racism. Smith called for an asset-based community mobilization.
What Can You Do:
Contact your state legislators to ask that Medicaid and health insurers fund the services of community health workers, doulas, recovery coaches and other important health care professionals in order to address health equity. These resources can save Black and Brown lives, and they need to be treated like the lifeline that they are.
For the complete discussion on “Racism and Health Care: What COVID-19 Has Exposed” click here for full video.
Some resources touched on by the panelists:
- The Philadelphia Study (by W.E.B. DuBois)
- Report of the Secretary’s Task Force on Black & Minority Health (The Heckler Report)
- Unequal treatment: Confronting racial and ethnic disparities in health care (Institutes of Medicine)
- National Association of Community Health Workers
Some resources to help you learn more about racism and health care:
- Why doesn’t the United States have universal health care? The answer has everything to do with race. (Jeneen Interlandi, 1619 Project)
- How racism is making us sick (TedMed Talk from David R. Williams)
- Allegories on race and racism (TedxEmory Talk from Dr. Camara Jones)
Some resources on being anti-racist
This article was previously post on Medium.com
Universal Health Care Foundation of CT fights on the front lines of health care activism and policy, because health care is a right everybody in Connecticut and beyond should enjoy. Join us here for more content and action opportunities.
This online discussion could not have been possible without the support and sponsorship of the William Caspar Graustein Memorial Fund, Connecticut Health Foundation, and The Donaghue Foundation. Thank you for being with us in the fight.
Back Issues

Developing a Research Agenda on High-Value, Equitable Care: The Power of Being Practical, Inclusive, and Innovative

The Room Where Research Happens: How I Became Part of a Group that Was Open to Research the Topic that Few Seemed Willing to Discuss