Practically Speaking
Winter 2019
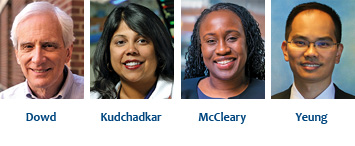
Greater Value Portfolio Awards
Donaghue has recently made four new awards from the fourth cycle of its Greater Value Portfolio program. This brings the total awards to 15, and more than $7.5 million has been invested in research that demonstrates new approaches to improved health care value. Two new requirements of the program are that a healthcare services organization must be a partner with the researcher and that the research question reflects strategic goals of that organization. Because the research will be closely aligned with the functions of a healthcare system, the timeline for the project was shortened to two years. The maximum allowable award for this year’s cycle was $440,000, which included a 10% indirect rate.
Bryan Dowd, PhD
University of Minnesota
“Incorporating Quality of Care Information into a Tiered Cost-sharing Health Insurance Benefit”
Partner organization: State of Minnesota
Tiered cost-sharing has the potential to realign both consumer and provider incentives in the U.S. health care system towards greater efficiency. Since 2002, the Minnesota State Employees Group Insurance Program has offered its 127,000 employees and dependents health insurance benefits through a system of primary care clinics placed in tiers based on total annual per capita risk-adjusted cost of care. Employees in choosing higher cost clinics face significantly higher deductibles and copays. Employees can access clinic quality information from Minnesota Community Measurement, but little is known about their use of these data or variation in quality across clinics or cost sharing tiers. The overall purpose of this study is to understand how best to incorporate information on clinic quality into this system. Specifically:
- How do employees use the quality of care information available under the current system?
- How could the system be improved?
- How does quality vary within and among tiers? Is there a cost-quality tradeoff?
- Would improved quality information affect providers’ efforts to improve quality?
Surveys, focus groups, and quantitative analyses will be used to answer these questions, and results will be shared with providers, the State of Minnesota employee health insurance division, and various policy-making communities.
Sapna R. Kudchadkar, MD, PhD
Johns Hopkins University
“Impact of a multifaceted early mobility intervention on clinical outcomes and ICU-acquired morbidities in critically ill children
Partner organizations: Johns Hopkins All Children’s Hospital, St. Petersburg, Florida; Our Lady of the Lake Children’s Hospital, Baton Rouge, Florida; Advocate Children’s Hospital, Park Ridge, Illinois
Recent decreases in pediatric intensive care unit (PICU) mortality rates have been offset by increased morbidity and length of stay for vulnerable young patients. Heavy sedation, bedrest, and delirium contribute to a PICU culture of immobility. While studies in adult ICU patients demonstrate the clinical benefits of early mobilization, fewer than 25% of critically ill children mobilize early in their PICU stay. We have demonstrated the safety and feasibility of the “PICU Up!” Mobility Program, which integrates sleep promotion, delirium prevention, and sedation optimization as a bundle to increase mobilization. However, the generalizability and broader impact on patient- and family-centered outcomes is unknown. The overall objective of this research is to determine the impact of a transdisciplinary and multifaceted early mobility program on clinical outcomes and ICU-acquired morbidities in critically ill children. Additionally, barriers and facilitators to high-performance bundle adoption in the three locations will be identified.
Nadine Jackson McCleary, MD, MPH
Harvard Medical School
“Assessing toxicity and adherence of oral cancer therapy with ePROs“
Partner organization: Dana Farber Cancer Institute
Cancer patients experiencing toxicity are less likely to adhere to potentially life-saving or life extending cancer directed therapy. We have mitigated this risk for patients receiving intravenous therapy, but a significant risk of toxicity and non-adherence remains for oral cancer directed therapy. In contrast to intravenous therapy, patients prescribed oral therapy are responsible for managing their own medication administration and safety. Suboptimal use of these treatments can lead to an increased likelihood of unplanned urgent visits to manage symptoms, diminished response to the therapy, and even death. The partnering healthcare institution has begun to address this gap by calling patients once after starting oral cancer therapy to conduct teaching and assess adherence. They have also successfully implemented electronic collection of patient reported outcomes during clinic visits to improve the capture of treatment-related toxicities. However, none of these efforts assess toxicity at home (where all oral cancer therapy is administered), evaluate adherence throughout the course of treatment, or integrate toxicity/adherence reporting with dedicated practice management efforts. To address these remaining gaps, this study will:
- Develop a robust, systematic program to expand electronically collected patient reported outcomes beyond during clinic visits to include collection of toxicity/adherence data between clinic visits for oral cancer therapy recipients (ePRO oral).
- Test the feasibility and patient and clinician acceptance of ePRO oral to improve oral cancer therapy safety and adherence among advanced breast or gastrointestinal cancer patients.
- Test the value of and potential barriers to ePRO implementation in oncology practice.
Kai Yeung, PharmD
Kaiser Permanente Washington Health Research Institute
“Value-based Formulary-Essentials: Testing and Expanding on Value in Prescription Drug Benefit Design”
Partner organization: Premera Blue Cross
The goal of this study is to improve value in pharmaceutical care by testing a promising drug formulary that aligns patient out-of-pocket costs for drugs with the drugs’ estimated value. The research team previously collaborated with Premera Blue Cross, the largest non-profit health plan in the Pacific Northwest, to evaluate a pilot version of this formulary. It reduced drug spending by 9%. The results informed Premera’s substantial redesign of the formulary (the Value-Based Formulary-Essentials or VBF-e). The VBF-e has now been implemented among 50,000 beneficiaries, a 10-fold increase in the uptake of the pilot. VBF-e will be assessed on (1) medication use, stratifying on whether cost-sharing for a drug increased or did not change with VBF-e; (2) spending by patients and by plan for drugs and non-drug medical care; and (3) emergency department use, hospitalizations and outpatient office visits. The results will help Premera to determine further modification of how drugs are categorized into tiers, changes to out-of-pocket costs associated with each tier, and decisions regarding wider implementation.